Adhesive Arachnoiditis: A Comprehensive Guide to Symptoms, Diagnosis, and Patient Safety
- EveBlackburn
- Dec 24, 2025
- 5 min read
Adhesive arachnoiditis is a rare but serious condition that affects the spinal cord. It involves inflammation and scarring of the arachnoid membrane, one of the protective layers surrounding the nerves of the spinal cord. This scarring can cause nerves to stick together, leading to chronic pain and neurological problems. Recognizing the symptoms early is crucial for managing the condition effectively and improving quality of life.
Understanding the Symptoms of Adhesive Arachnoiditis
The symptoms of adhesive arachnoiditis can vary widely depending on the severity and location of the inflammation. Many people experience a combination of symptoms that worsen over time. Common signs include:
Chronic pain: This is often the most prominent symptom. The pain can be sharp, burning, or aching and may radiate down the legs or arms.
Numbness and tingling: Patients often report a "pins and needles" sensation or numbness in the affected areas.
Muscle weakness: Weakness in the legs or arms can develop, making walking or using the hands difficult.
Bladder and bowel dysfunction: In severe cases, nerve damage can affect bladder and bowel control.
Spasms and cramps: Muscle spasms and cramps are common and can be painful and disruptive.
These symptoms can mimic other spinal conditions, which sometimes leads to delayed diagnosis. If you experience persistent or worsening neurological symptoms, it is important to seek medical evaluation.
Causes and Risk Factors
Adhesive arachnoiditis is often caused by injury or irritation to the spinal cord's arachnoid membrane. Some common causes include:
Spinal surgery or trauma: Surgical procedures or injuries to the spine can trigger inflammation.
Infections: Bacterial or viral infections affecting the spinal cord may lead to arachnoiditis.
Chemical irritation: Exposure to certain chemicals during spinal injections or contrast dyes used in imaging can cause irritation.
Chronic inflammation: Conditions that cause ongoing inflammation in the spine may increase risk.
Understanding these risk factors can help in prevention and early detection. If you have a history of spinal surgery or injury and develop new neurological symptoms, it is important to inform your healthcare provider.
Diagnosing Adhesive Arachnoiditis
Diagnosing adhesive arachnoiditis involves a combination of clinical evaluation and imaging studies. Here’s what to expect:
Medical history and physical exam: Your doctor will ask about your symptoms, medical history, and perform a neurological exam to assess strength, sensation, and reflexes.
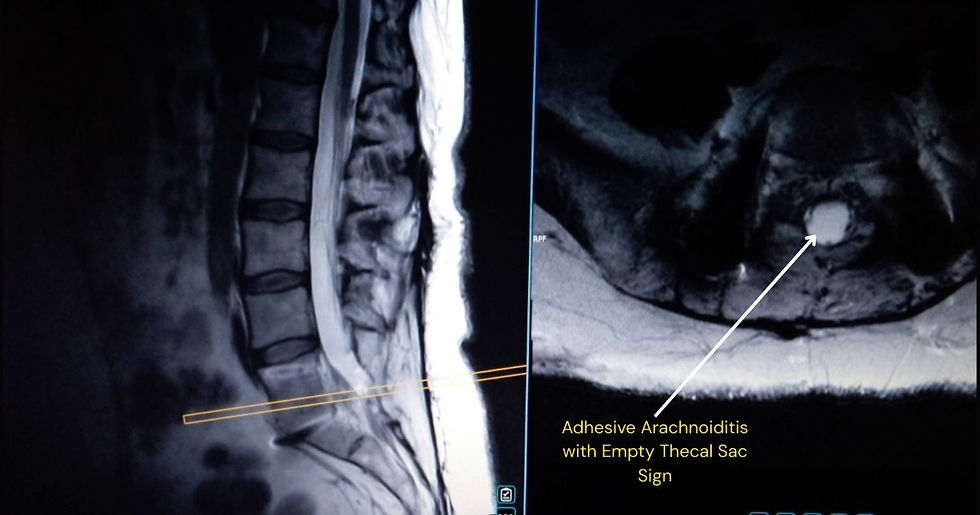
Magnetic Resonance Imaging (MRI): MRI is the most effective tool for visualizing inflammation and scarring around the spinal cord. A high-resolution MRI of the Lumbar Spine (without contrast) is the gold standard for diagnosing Adhesive Arachnoiditis, as it clearly shows nerve root clumping and peripheral displacement (the 'empty sac' sign). While some doctors request contrast, it is often unnecessary for a diagnosis and carries its own risks.
Myelogram: Historically used for spinal imaging, a Myelogram is strongly discouraged for anyone suspected of having Arachnoiditis. Not only does the required lumbar puncture pose a significant risk of triggering or worsening the disease, but the contrast dye itself can mask the nerve root adhesions, making an accurate diagnosis more difficult. A specialized MRI is a safer and more effective alternative.
Electromyography (EMG): EMG tests nerve and muscle function to assess the extent of nerve damage.
Early diagnosis is key to managing symptoms and preventing progression. If you suspect you have adhesive arachnoiditis, ask your doctor about these diagnostic options.

Managing and Treating Symptoms
Managing Adhesive Arachnoiditis: What Works and What to Avoid
While there is currently no cure for Adhesive Arachnoiditis (AA), the goal of treatment is to suppress neuro-inflammation, manage pain, and improve daily functioning. However, because AA is an inflammatory disease of the spinal canal, traditional "back pain" treatments are often dangerous for our community.
Pain & Inflammation Management: The cornerstone of treatment is a specialized protocol combining anti-inflammatory drugs, neuropathic pain relievers, and muscle relaxants. We focus on calming the "fire" in the spinal canal rather than just masking the pain.
Explore more: [Treatment Options Page] and [Alternative Treatment Page]
Physical Therapy & Aquatherapy: Mobility is medicine, but it must be gentle. Tailored exercises help maintain strength without overtaxing the nervous system. Aquatherapy is highly recommended; the buoyancy of water reduces gravitational pressure on the spinal cord, allowing for movement that would be too painful on land.
WARNING: Nerve Blocks and Injections: Unlike standard care, epidural steroid injections (ESIs) and nerve blocks should be avoided. These procedures carry an FDA "Black Box" warning and are specifically contraindicated by manufacturers like Pfizer (Depo-Medrol). While the FDA officially identified 41 cases of Arachnoiditis linked to these injections, the actual number is likely significantly higher due to systemic under-reporting by medical facilities.
Take Action: If you have been injured by an ESI, you can report it directly to the FDA. Your report helps break the silence and protect others.
Surgical Options: Surgery is rarely recommended and should be considered a last resort. Entering the spinal canal often triggers more inflammation and creates additional scar tissue (fibrosis). Most experts agree that attempting to "clean out" adhesions usually results in the body producing even more aggressive scarring, leading to permanent disease progression.
Lifestyle Modifications: Success often comes down to daily choices. Maintaining a healthy weight, practicing neuro-protective pacing (avoiding "boom and bust" cycles), and using assistive devices can significantly improve quality of life and prevent debilitating flares.
It is important to work closely with a healthcare team to develop a personalized treatment plan. Support groups and counseling may also help cope with the emotional impact of chronic pain.
When to Seek Medical Help
When to Seek Immediate Medical Attention
If you experience any of the following "red flag" symptoms, seek a medical evaluation promptly:
Sudden or Worsening Weakness: New or progressing loss of strength in the legs or arms.
Loss of Bladder or Bowel Control: Any new changes in function or sensation.
Severe, Unrelenting Pain: Pain that is atypical or does not respond to your rescue medications.
Spreading Numbness: Tingling or loss of sensation that intensifies or moves to new areas.
Taking the Right Next Steps
While timely care is vital, it must be the right kind of care. To ensure you receive the safest and most effective treatment:
Start Here: Visit our Starting Point page for a roadmap on navigating a crisis or new diagnosis.
Consult Specialists: Use our Physician List to find doctors who specialize in diagnosing and treating Arachnoiditis.
Be Your Own Advocate: Recognizing these signs empowers you to seek proactive care. Education is the first step toward living better with Adhesive Arachnoiditis.
Protect Your Spine: Download the Patient Advocacy Sheet
In the exam room, knowledge is your best defense. Many healthcare providers are unaware that standard "back pain" treatments—like Epidural Steroid Injections (ESIs)—carry FDA Black Box warnings and can cause or worsen Adhesive Arachnoiditis.
We’ve created a professional Medical Alert & Advocacy PDF to help you bridge the communication gap. This one-page document outlines:
Official FDA warnings and manufacturer contraindications.
The risks of "routine" spinal entries (lumbar punctures and epidurals).
Evidence-based clinical recommendations for safer care.
Don't go to your next appointment alone. Download, print, and hand this sheet to your medical team to ensure your history of Arachnoiditis is respected and your spine is protected.
Help Us Break the Silence
By sharing this information, you aren’t just spreading awareness—you are potentially providing the 'missing piece' to someone whose life has been changed by an unrecognized injury. To make sharing even easier, we have created a Social Media Toolkit filled with ready-to-use graphics, captions, and hashtags. Please share this post and use the toolkit to help us demand safer medical standards and protect our community.
Coming Soon: A Deep Dive into Spinal Entry Risks
We are currently developing a dedicated blog series that will take an in-depth look at:
The "Black Box" Reality of ESIs
Why Epidurals and Lumbar Punctures are High-Risk for AA
How to Safely Refuse or Navigate Necessary Spinal Entries
Join the Movement: Connect with ACMCRN
Follow our official channels to stay updated on these upcoming articles and community events:



Comments